Trial Magazine
Theme Article
A Picture Is Worth 1,000 Words
To help jurors understand your client’s losses, incorporate a wide range of witnesses and exhibits into your trial damages presentation.
February 2022When presenting proof of damages, we owe it to our clients to submit evidence of all the injuries they have suffered. When I speak to jurors about damages, I paraphrase David Ball1 and talk about three kinds of harms and losses: harms that can be fixed, including economic losses such as lost wages and medical bills; harms than can be helped, including through medical procedures, adaptive devices, and personal assistance; and harms that cannot be fixed or helped, including noneconomic losses such as the lost enjoyment of life, loneliness, isolation, and chronic pain.
No magic formula exists for identifying and proving damages in your case. Plaintiff attorneys must develop damages from intake through closing argument. And at trial, focus every discussion of damages on helping jurors identify and empathize with your client’s three kinds of harms and losses. To do this, introduce a range of witness testimony and evidence, much of which will build on and corroborate each other. You need to convince the jurors of the injury, as well as its severity and lifelong impact on your client. Here are several tools to help jurors better understand your client’s losses.
Treating Physician Testimony
Your client’s treating physician may be the best witness to establish the nature and severity of your client’s injuries. As opposed to experts, who might be seen as “hired guns,” jurors may view treating physicians as unbiased and give their testimony more weight.
Primary care physicians often have a significant history with the patient and can provide an unbiased history of the client’s health. These doctors can corroborate your client’s testimony about pre-injury activities and abilities, confirm your client’s ongoing deficits, and refute any defense allegations of malingering. They also can provide unbiased documentation of the cause of the injury, as well as the long-term effects that the injury will have on your client.
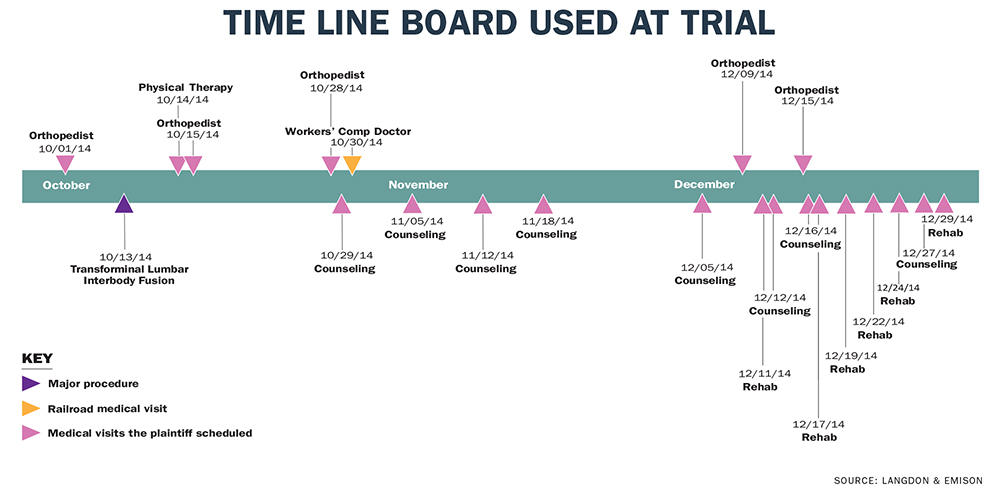
For instance, in one case I handled, a young railroad engineer was injured on the job. At trial, the railroad hotly contested the nature and extent of the harm. The railroad went as far as arguing in closing that our client was lying about his severe injuries. We dedicated a large portion of the trial to evidence of those injuries. We focused on evidence from our client’s physicians, including several whom the defendant railroad had approved or even provided. We highlighted that our client had over 220 medical visits for his injuries and created a time line of those visits. We blew up 15 time line slides showing all the visits and lined the courtroom with them.
You also should use testimony from treating physicians to undermine allegations of malingering and exaggeration of injury. In the railroad case, we asked each treating physician, including those hired by the railroad, whether our client was exaggerating his symptoms, and each confirmed the injuries were not exaggerated.
We also relied on medical reports from the railroad’s doctors, who identified the workplace injury as the cause of our client’s ongoing medical issues. Importantly, the railroad’s chief medical officer found that our client was not medically qualified to continue in his employment.
Specialty Evaluations
Treating physicians may limit their focus to identifying and treating your client’s immediate injury, and they may not be comfortable opining on the long-term consequences of the injury. In such cases, seek out a medical specialist who can provide a detailed evaluation of your client’s injury and effectively communicate that to the jurors. Medical specialists can take the witness stand and teach the jurors the medicine necessary to understand your client’s injuries and ongoing physical limitations.
For instance, in an auto collision case, we used an orthopedic surgeon to educate the jurors on our client’s cervical spine injuries. This specialist was able to explain how a relatively slow speed auto collision can cause injury to the spine and how he could determine that trauma from the crash caused the injury as opposed to ordinary degenerative changes from aging.
Specialists also can directly address your client’s damages in ways that a treating physician may be unable to do. Our orthopedic specialist educated the jurors about the long-term effects from the cervical fusion that our client underwent. The specialist explained how fusing the injured vertebra put additional strain on vertebra above and below the fusion and how our client would become progressively more limited in her motion, particularly in her ability to turn her neck from side to side. This testimony helped the jurors understand the true severity of the injury beyond the date of the reparative surgery.
And specialists can complement the treating physicians’ testimony to explain the causation, nature, and extent of an injury. Specialists can look beyond treatment and analyze the facts surrounding the injury. They can then tie these facts about your client’s injury to the defendant’s conduct. For example, in the auto collision case discussed earlier, the treating physician described our client’s injuries and the surgery and recovery she underwent. Our orthopedic specialist was able to rely on and comment on the treating physician’s work and also further explain the mechanism of injury from the crash forces, as well as the likelihood of additional future complications and treatment.
The saying that a picture is worth 1,000 words is certainly true for medical evidence.
Medical Illustrations and Animations
The saying that a picture is worth 1,000 words is certainly true for medical evidence. Medical illustrations and modeling are incredible tools to help jurors understand very complex medical testimony and procedures. They can range from simple drawings by the treating physician or expert to customized illustrations of your client’s injury or medical procedure to fully interactive 3D modeling. These tools allow your medical witness to become a professor, instructing jurors on how the injury occurred, why a corrective procedure was required, what effect the injury has had on your client’s life, and how and why your client will continue to suffer pain in the future.
For instance, in one case in which my client, a young child, was very badly burned in a car crash, I used customized medical illustrations to explain the numerous procedures he had to endure. The illustrations showed the jurors the extent of his injuries—he received skin grafts on a large portion of his body, had dead muscle removed from his legs, and had his right arm amputated. These illustrations, along with a time line of procedures, helped convey to the jurors the months of torture this small child experienced just to survive.
In the railroad workplace injury case described earlier, my client suffered continued back pain even after a transforaminal lumbar interbody fusion.2 I worked with my medical expert and a spinal surgeon, using an interactive 3D model, to help the jurors visualize and understand the invasiveness of the surgery and the hardware that remained implanted in my client’s spine. The doctors maneuvered the 3D model in real time on the witness stand to describe the procedure. The physicians also used the modeling program to remove various elements (such as muscle and bone) and highlight the surgical hardware, including the large screws embedded in my client’s vertebra.
Life Care Plans
In every discussion of damages at trial, address those damages likely to occur in the future. You often can prove future damages through the testimony of a life care planner or a similar expert.3 Life care planners are medical professionals—typically doctors, nurses, or rehabilitation therapists—who identify future needs created by an injury or disability. They can develop an integrated plan for the care, equipment, and other services required to meet the injured person’s medical and safety needs. This plan allows jurors to understand the costs associated with treating the injured plaintiff over the course of his or her expected lifetime.
A life care plan generally includes the following categories of care and services:
- physician care
- medical procedures and hospitalizations
- labs and diagnostics
- psychological care
- rehabilitation and therapy
- medications
- medical supportive care
- adaptive equipment and home modifications
- medical supplies
- vocational training
- household services
- transportation.
Life care plans typically are used in large, catastrophic injury cases, but they also can be very useful in cases involving less severe injuries. My firm frequently uses life care plans in smaller cases when the current medical expenses are low but treatment is expected to continue. Submitting a life care plan with current medical bills to an adjuster early in the litigation allows the insurance carrier to properly value the case and greatly improves the likelihood that the case will resolve for the full value of the claim.
Lay Witnesses
Developing damages requires you to show the jurors that your client was injured and how those injuries affect your client every day. Lay witnesses such as family members, coworkers, or clergy can bridge the gap between the medicine and your client. Frequently, they can paint a picture of your client’s pre-injury activities and abilities and contrast those abilities with the deficits experienced after the injury. And effective use of stories and anecdotes can humanize and personalize your client to jurors while confirming the medical findings.
Lay witnesses, such as your client’s spouse or loved one, can communicate your client’s losses to the jurors. But beware that although these witnesses may provide detailed testimony about your client’s injuries and impairment, the jurors may see them as biased.
Another option is an independent and objective lay witness who can corroborate and reinforce the testimony of your client and their loved ones, helping to persuade the jurors of the nature and extent of your client’s injuries. Objective lay witnesses include clergy members, professional colleagues, or other acquaintances who have nothing personally to gain from their testimony.
In some cases, it may be appropriate to document your client’s daily struggles using documentary videos. A video of your client’s day can highlight many of the greatest challenges your client faces when dealing with his or her injury. Such videos can give the jurors a first-hand perspective of your client’s deficits and permit them to see exactly what limitations have been caused by your client’s injuries. These videos can be authenticated by the documentarian, the client’s family members, or your client.
Starting from case intake, frequent discussions with your client and his or her family help you identify critical witnesses who can provide evidence of harms and losses. Medical expert, life care planner, and lay witness testimony can communicate the nature and extent of all your client’s losses—including future ones—to the jurors. Combining this testimony with graphics showing your client’s struggles
helps ensure that the wrongdoer is held responsible.
Brett A. Emison is a partner at Langdon & Emison in Lexington, Mo., and can be reached at brett@lelaw.com.
Notes
- David Ball, David Ball on Damages 3 (3d ed. 2012).
- A transforaminal lumbar interbody fusion is a surgery to reduce pain and nerve irritation by stabilizing the spinal vertebra and the disk that provides cushion between the bones. The surgery fuses adjacent vertebra by creating solid bone where the disk had been and eliminates movement between the vertebra.
- For more on life care plans, see Nancy Bond, Hiring a Life Care Planner, Trial, April 2017, at 49; David L. Kwass & Elizabeth Bailey, Protect Your Life Care Plan, Trial, April 2017, at 52.
Toolbox for TBI Cases
Damages caused by a traumatic brain injury (TBI) are frequently disputed, often because defendants believe TBIs are merely subjective injuries and thus damages may be difficult to measure objectively. A TBI occurs when sufficient force to the head causes some change in neurologic function. Mild traumatic brain injuries (mTBIs)—which include concussions or even milder blows to the head—have been called a silent epidemic. Most of the millions of patients who visit emergency rooms (ERs) each year with mTBIs are simply treated and released.1 But studies have shown there is nothing “mild” about an mTBI—a significant number of mTBI victims will suffer long-term effects, including headaches, blurred vision, memory loss, impulsiveness, mood disorders, and personality changes.2
Tragically, the Centers for Disease Control and Prevention found that mTBIs are vastly underreported, with one study estimating that 60% go undiagnosed.3 Another study found that ERs fail to diagnose more than half of TBIs.4
Identifying an mTBI. To identify clients who might have suffered an mTBI, look first at the incident report or initial medical records following the injury.5 Although a TBI (including an mTBI) can occur even without a loss of consciousness, any report of loss of consciousness is a tell-tale sign.
Your clients likely will be poor historians of their injury and unable to tell you if they lost consciousness and, if so, for how long. Instead, develop this evidence with scene witnesses and emergency responders, and tailor your investigation to each scene. In an auto collision, for example, evidence of a TBI could include signs that your client struck his or her head—look for evidence of spidering on the windshield, denting on the steering wheel, or bruising on your client’s head. Your client might also report headaches, dizziness, memory loss, or other signs of a TBI.
When your client has little evidence of physical injury, your biomechanical or accident reconstruction expert can provide critical testimony. For example, a biomechanical expert may be able to identify more than one head strike during an auto collision. A biomechanical or accident reconstructionist also can calculate the crash forces experienced inside the vehicle during the collision. In many crashes, the calculated crash forces on occupants far exceed the human brain’s tolerance.6
Specialists such as neurologists or neuropsychologists often can identify a TBI. A neuropsychologist can conduct testing that may identify cognitive deficits following a TBI. A neurologist can conduct diagnostic examinations that identify structural injuries to the brain and neurologic pathways.
Do not be discouraged by negative diagnostic tests. Although neuroimaging technology is constantly improving, CT scans, for example, are poor identifiers of TBIs because they can only identify bleeding and fractures. Other, more complex tests (such as perfusion imaging or diffusion tensor imaging) may show structural changes. But many times an mTBI is associated with normal structural neuroimaging findings.
Although a negative diagnostic test will not exclude the possibility of an mTBI, a positive neuroimaging finding can be critical evidence and help the jurors understand the significance of the injury. Your expert will use the neuroimaging to describe the structural damage to the brain and show the jurors exactly what areas of the brain have been injured and tie those injuries to ongoing, documented neurological impairments. Your neuroimaging expert also can use the findings to corroborate other neuropsychological testing and reported cognitive deficits. This evidence can be vitally important, assisting the jurors in understanding the significance of the brain trauma.
Focus on deficits. In any case involving TBIs, do not exaggerate the severity of the injury or try to find evidence that the injury was more severe than it was. Instead, focus on the deficits you can document. Our office, for example, represented an Army helicopter pilot who suffered an mTBI in an auto collision when his vehicle overturned after being struck on the highway. He lost consciousness briefly and suffered seizures at the crash site and again en route to the hospital.
At trial, someone observing our client likely would not have known he was injured. So instead, we focused on contrasting his abilities before and after his injury, urging the jurors to concentrate on the deficit our client suffered. His job as a military helicopter pilot and instructor required extreme focus and mental precision, which he was no longer able to maintain after the crash; moving a helicopter throttle half-an-inch equates to hundreds of yards on the ground and the difference between life and death on missions. We also highlighted the variance of his tests. He had an immediate recall of 75% but a delayed recall of just 37%, which showed that he lost nearly half of his ability to recall information over time.
During the trial, the defense accused our client of lying and making up his injuries. We combated this by relying on multiple pieces of evidence proving the injury—we used cognitive testing showing deficits, as well as our accident reconstructionist to explain how the injury could occur. This expert was an engineer, not a medical doctor, so the court would not let him testify that the crash caused a TBI, but it let him testify about the forces exerted in the crash—and that they were four times the amount necessary to cause a TBI.
We also had highly trustworthy lay witnesses, including a police officer and a sitting appellate court judge, testify about the neurological deficits they observed in our client since the crash. All this evidence was critical in overcoming the defense claim that our client was making up his injuries.
Notes
- See Ctrs. for Disease Control & Prevention, Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation, at 6 (2014), https://tinyurl.com/42fux8tr.
- Ctrs. for Disease Control & Prevention, Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem (2003) (75% of TBI are categorized as mTBI). See also id.; Ctrs. for Disease Control & Prevention, Heads Up; Facts for Physicians About Mild Traumatic Brain Injury (MTBI), at 2 (2009) https://stacks.cdc.gov/view/cdc/12340.
- Page Walker Buck, Mild Traumatic Brain Injury: A Silent Epidemic in Our Practices, 36 Health & Social Work 299, 301 (Nov. 2011); Wesley Rutland-Brown et al., Traumatic Brain Injuries After Mass-Casualty Incidents: Lessons From the 11 September 2001 World Trade Center Attacks, 22 Prehospital & Disaster Medicine 157 (June 2007).
- See Janet M. Powell et al., Accuracy of Mild Traumatic Brain Injury Diagnosis, 89 Archives of Physical Medicine Rehabilitation 1550, 1552 (Aug. 2008). (This study primarily looked at mTBIs.)
- AAJ’s Traumatic Brain Injury Litigation Group has additional resources for handling these cases. Go to www.justice.org/litgroups to learn more.
- The brain is most susceptible to injury caused by rotational motion. An angular acceleration of just 6,000–9,000 rad/s2 is sufficient to bruise the brain. See, e.g., Svein Kleiven, Why Most Traumatic Brain Injuries are Not Caused by Linear Acceleration but Skull Fractures Are, 1 Frontiers in Bioengineering & Biotechnology 7, 15 (2013).

